A Functional Medicine Dietitian's Approach to Breast Cancer Prevention (Part 2)
I am a functional medicine dietitian who was diagnosed with breast cancer at age 31 years old.
Part 1 of this blog post outlines how I found my cancer and advocated for myself (which saved my life!) and how I integrated holistic modalities and alternative practices into my care plan to improve my quality of life and expedite my healing.
I am writing this post in 2024, almost five years after my diagnosis and double mastectomy.
My treatment plan has changed over the last few years. At first my focus was recovering from surgery and rebuilding my strength. Now I have gained even more insights into my health and my focus has shifted to prevention.
In this post I share integrative modalities I’ve taken to support myself and prevent breast cancer recurrence.
How and why I decided to go off of Tamoxifen (my cancer preventing medication).
I share my own story about heavy metal poisoning and environmental exposures, and how to support their detoxification!
Nutritional support strategies - Foods to focus on for breast cancer prevention, including evidence based functional foods.
Fasting strategies to prevent tumor formation and promote cellular health.
Supplement strategies for breast cancer prevention and detoxification.
No cancer journey is the same, and creating a wellness plan for cancer is a highly individualized process because:
Every person’s body is different, even without a cancer diagnosis. Each person has different symptoms, different underlying imbalances, unique lives and clinical needs.
The nature of different types of cancer will respond to different therapies - for example breast cancer is metabolically different from brain cancer or prostate cancer, and therefore need a different approach. Even two breast cancer diagnoses can be metabolically different and require different therapies.
Depends on what stage of treatment a person is undergoing. Surgery recovery requires a different approach from chemo and radiation.
Many supplements and nutritional approaches are contraindicated during chemo and/or radiation. This is because chemotherapy is intentionally stressful on the body, and kills cells with high turnover (which is why many people have digestive issues, hair loss, etc). Most antioxidants and supplements will counteract these therapies, and should be considered only after treatment is over and approved by an oncologist. Instead of cancer prevention, the goal of nutrition during chemo or radiation is to reduce side effects and discomfort as much as possible to improve a person’s quality of life.
The approach changes again when an individual has ‘no evidence of disease’, has completed active treatment, and / or is in remission. The focus then can shift to cancer prevention, which is when personalized antioxidant regimens and metabolic support can be helpful.
This article is purely educational. Remember that each cancer journey is so different. Any medical decisions should be discussed with your doctor.
Hormone Suppressing Medication
My journey on Tamoxifen
I was diagnosed with stage 1 breast cancer (invasive ductal carcinoma), which means the cancer was localized to my breast and had not spread into my lymph nodes. While my surgeon removed all cancerous tissue along with my breast tissue and achieved ‘clean margins’, I still required additional medical treatment.
I was diagnosed with hormone positive cancer, meaning that the tumors grew in response to estrogen and progesterone. Therefore my oncologist recommended an extremely common medication called “Tamoxifen”. Tamoxifen is a hormone blocker that prevents estrogen and progesterone from binding to cellular receptors, therefore inhibiting the growth of hormone sensitive tumors.
Tamoxifen is typically prescribed for 5-10 years depending on an individual’s risk for recurrence. Depending on a variety of calculations, oncologists may also add additional hormone suppressing medications like Lupron.
Of course I didn’t want my cancer to return and I was theoretically behind this. However, after a few months of taking Tamoxifen I started experiencing unbearable side effects.
Tamoxifen put me into early menopause. My doctor explained that this would probably be temporary because I was so young.
That concerning fact aside, I was not prepared for the severity of the side effects I experienced. According to my doctor some of the issues I experienced, like weight gain, were common. But other side effects like neuropathy only happened to 1% of those taking Tamoxifen. When I was experiencing these wild side effects I searched the internet high and low for others like me, without success. I am sharing this in hopes that it will reach someone else who is struggling.
Hot flashes and night sweats - this is very common in perimenopause and a very common side effect of Tamoxifen. Hot flashes often happen because of fluctuating estrogen levels. There are some things that were immediate hot flash triggers for me, like 1) Exposure to heat (like opening the oven). 2) Alcohol intake (even after a few sips of wine) and 3) feeling emotional, whether I got excited or upset. I struggled to sleep through the night because of severe hot flashes that would make me sweat through my PJs, and oftentimes even my sheets! The lack of sleep increased my anxiety and made me feel hopeless and depressed.
Weight gain - I gained 40 pounds as a side effect of Tamoxifen. All the studies I have seen online reported an average gain of 10-15 pounds, and I was astonished that my body blew up so much. Regardless of what I did with my nutrition I steadily gained weight over the 3.5 years I stayed on the medication, and it completely melted off once I discontinued it.
Changes to my bloodwork. My blood work also reflected that I was becoming insulin resistant (which is a fancy word for uncontrolled blood sugar, which precedes pre-diabetes). This was incredibly alarming to me because I didn’t want to trade one disease in for another. After further investigations, I found research linking the use of Tamoxifen and the development of insulin resistance.
Neuropathy - I began to lose sensation in my hands and my feet. Apparently this happens to only 1% of people on Tamoxifen. My integrative psychiatrist recommended high dose fish oil, which slightly improved the symptoms but it persisted throughout my time on Tamoxifen.’
Every time I visited my oncologist, I begged her to take me off Tamoxifen.
She tried to prescribe a drug called Effexor to manage the hot flashes, however I was extremely resistant. A friend of mine had started on Effexor a few years earlier. About 72 hours on the drug she developed permanent tinnitus and hearing impairment. While this is admittedly an extremely rare side effect, I wasn’t willing to take the risk.
At first we tried halving my dose of Tamoxifen, which was somewhat helpful. The night sweats calmed down enough for me to sleep and feel like a somewhat sane human, however the hot flashes, weight gain and neuropathy persisted.
We eventually ran a test called “Breast Cancer Index” to help me make a choice about Tamoxifen. The Breast Cancer Index dissects the tumor and evaluates the risk of recurrence after five years of tamoxifen, and is based on a variety of factors. I pushed to run this test earlier than was typical in order to help me make this medication choice. If I had an extremely high risk I would bear the side effects for another 18 months.
My breast cancer index came back extremely low. I shed a few tears and did a little happy dance. If I continued Tamoxifen I would have a 3% risk of recurrence between years 6-10 and the risk would continue to decrease with time. If I discontinued it at 3.5 years like I wanted to, my risk would probably be around double at 6%.
My oncologist told me that “Anything under 10% is extremely ideal” and that my risk of recurrence was very low.
While I wanted to do everything in my power to prevent my cancer from returning, I also knew the lack of sleep, emotional turmoil and quality of life mattered in terms of my stress levels and health too. Chronically elevated cortisol suppresses immune cells that fight tumors. I weighed all of these facts when making a choice about what to do. I made it 3.5 years, and the statistics ultimately provided me enough confidence to discontinue the medication.
I also turned to functional medicine modalities to provide additional support.
How environmental toxins are linked to cancer
Functional medicine is always seeking to understand the underlying causes of disease and imbalances.
Environmental risks and exposures have grown exponentially over the years, and so has the rate of breast cancer in women under 40. The two are connected - many pollutants are carcinogens and endocrine disruptors and increase the risk of breast cancer.
This can feel disheartening to hear, however I always think that there are empowering steps we can take. Reducing our risk of cancer related to environemntal exposre requires a two fold approach:
Reduce exposure when possible
Optimize our body’s detoxification pathways
Reduce your exposure to environmental toxins:
Drink filtered drinking water. I recommend an under the sink filter like this one from aquasana or a berkey filter. Note: the only reason I don’t recommend reverse osmosis is because it wastes a lot of water and strips the minerals away.
Always use glass or stainless steel for bottles and tupperware
Never heat anything in plastic. Also consider the tops of your to-go coffee and tea cups (the hot liquid passes through plastic, which releases microplastics), and even consider the use water bottles on a hot day.
Eat organic produce, when possible. If you are on a budget or have limited access, follow the clean 15 and dirty dozen lists.
Evaluate your cosmetics and swap out ones that contain toxins like phthalates and PCBs. EPA’s Skin Deep is a great resource for finding clean cosmetics and skincare products.
It is also important to understand that our body’s detoxification pathways are constantly working for us. I get into ways we can optimize these pathways in the below section, however it is important to know that the body is constantly working for us every second of the day!
The liver processes harmful compounds (these can be ingested compounds or byproducts from healthy metabolism, like hormones). These compounds are then eliminated. Major routes of elimination include:
Digestive tract - via stool
Kidneys - via urine
Skin - via sweat
Lungs - via breath
If our exposure to toxins exceeds the body’s detoxification capacity, we will likely experience symptoms such as poor immunity, autoimmune conditions, fatigue, weakness and even the development of cancer.
My cancer diagnosis was the only sign of heavy metal exposure I had …
How to detoxify heavy metals and environmental toxins to reduce cancer risk
My breast cancer diagnosis is linked to environmental health issues. I grew up in downtown Manhattan and was 13 years old on Sept 11. When the twin towers fell, ten thousand tons of asbestos and other toxins like dioxins, PCBs and heavy metals were released into the environment. At first the EPA told us to not worry and that it was safe to continue living downtown, but in the years following the attacks we discovered the true impact of these airborne toxins on our health.
My mother and I, along with 400,000 workers, residents and survivors were exposed to toxic contaminants that increased risk for illnesses, including cancer. If you are interested in learning more about this, here’s a link that dives into the environmental impact of 9/11.
This exposure impacted my mother first and then me. In 2013 my mom passed away of lung cancer, a documented 9/11 related illness. Then, as you already know, I was diagnosed with breast cancer in 2019 at the age of 31. Both lung and breast cancer are among the most common diagnosed cancers in 9/11 survivors.
I knew my 9/11 exposure increased my risk for developing cancer, but life happens and it took me years to address this piece of my health. Finally, discontinuing tamoxifen was the wake up call I needed to address this.
I ran two different toxin profiles:
Heavy Metal toxin profile via Doctor’s Data
Environmental Toxin test via Vibrant America
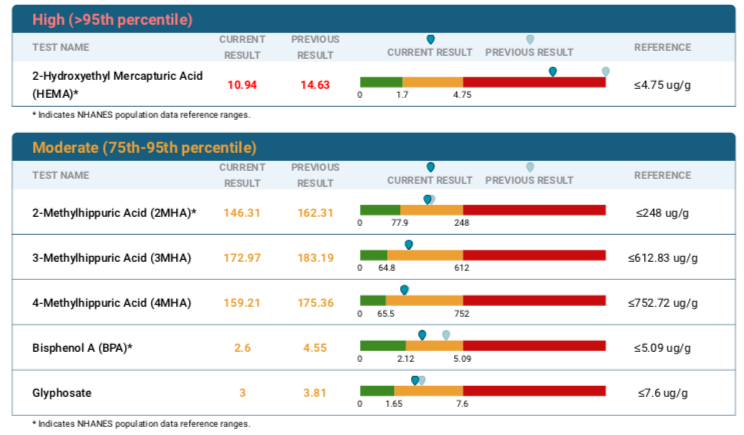
My test results showed alarmingly high levels of mercury and lead, along with another environmental toxin called 2-Hydroxyethyl Mercapturic Acid (HEMA). See below for my results!
Once I identified the heavy metals and had my starting data, I embarked on a comprehensive detoxification program.
Chelation therapy is the centerstone for heavy metal detoxification. The body stores heavy metals in organs and tissues, and therefore need to be drawn out with chelators which bind them and help your body eliminate them. In addition to chelation, it is essential to support major routes of detoxification (especially liver, gut, kidneys, skin) so that the toxins are not reabsorbed. For example, detoxification while having digestive issues or constipation will be counterproductive because the gut will send toxins back to the liver if there’s nowhere for them to go. We need to clear the detoxification pathways so the toxins have a way to leave!
Chelation can be done on IV or through oral medication. When it comes to detoxification, I believe slow and steady is always best, which is why I would recommend oral over IV chelation.
My doctor prescribed a chelation compound called “DMSA”, however there are others available depending on the type of metals you are targeting. There are accounts online about using whole foods
Days 1-3 take 500 mg DMSA three times per day
Days 4-14 discontinue DMSA
Repeat for 5 rounds
Like other environmental toxins, HEMA does not require chelation therapy but we were targeting this exposure by optimizing detoxification at whole.
At the time of writing this I have undergone a 3 month chelation protocol. I am happy to report that my mercury levels have plummeted, my lead levels have halved and my HEMA exposure has gone down 4 points. I still have work to do, and will likely do another round of chelation therapy and supportive detoxification practices. But it is good to pause and take inventory of my progress in order to see the efficacy of the practices I am doing and if I need to pivot.
Here are the test results side by side, a few months and one round of chelation / detoxification in between. I will likely do another round of detox support, and hopefully see all the numbers within an acceptable range.
Heavy Metal Results:
Initial test results (July 2023)
Follow up results (April 2023) - as you can see the mercury and lead along with several other toxins came down!
Note the time lapsed between the two tests is related to overseas travel. I left the country several times in 2023 and needed to be home for a solid 3 months to follow the proper protocol!
Environmental Toxin Results
This test lists the side by side values - see current results and previous results to see how much these decreased. There wasn’t as dramatic as a reduction, which indicates I will need to continue with the infrared sauna and detox support formulas that I share below.
Supplement to support detoxification.
Supplements can be incredibly helpful for supporting liver and gut health, which are key for optimizing detoxification capacity. However, supplements are unregulated in the US and quality and dosing varies widely. Follow this link to access the protocol for the below supplements, including brands and dosing. You can make an account on fullscript without purchasing anything.
In the spirit of full transparency, I do receive a small kickback on supplements sold through my online dispensary.
B complex vitamins - required for liver detox and often depleted with stress and alcohol
Liver support formula - herbal supplement that contains bioactive ingredients like milk thistle, and dandelion to improve whole body antioxidant capacity and liver health.
Detox support formula - contains functional ingredients like Curcumin, taurine and broccoli sprouts as well as milk thistle supports detoxification. Compliments the liver support formula well.
Flaxseeds for fiber and digestive regularity
Sunfiber for fiber and digestive regularity
Vitamin C - supportive antioxidant
holistic practices that support detoxification:
Infrared sauna -is best for targeting fat soluble environmental toxins. Although the research doesn’t show benefit for the use of infrared sauna on heavy metals, the functional medicine perspective emphasizes the need to optimize routes of detoxification to reduce whole body burden. Sweat is a major route of detoxification, and clearing other toxins support our systems for removing lead and mercury.
Colonics - on day 3 or 4 of every chelation round (every 2 weeks), to reduce the chance of reabsorption. Like I mentioned above, the gut is a major route of detoxification. Constipation, and even incomplete elimination, increases the risk of reabsorption. Think of colonics as exercise for your colon - it stimulates the contraction of the smooth muscles that line the gut to get things moving out. This should only be done by a RN who is a certified colon hydrotherapist.
Castor oil packs - placed on the liver.
Rebounder - 10-30 minutes a day gets lymph flowing!
Skin brushing
Tongue scraping
Oil pulling
How to eat for breast cancer prevention
Food is the foundation for health.
There are specific areas we can focus our energy to fortify the immune system, support a healthy detoxification and also a healthy metabolism to prevent tumor formation. When considering optimal foods for cancer prevention, here are some areas I focus my energy:
Ensure adequate protein. Every cell in our body requires high quality protein to function properly. Protein is not only essential for strength and muscle mass but also to support the immune system and liver detoxification that removes harmful compounds. Quality matters. Optimal sources: wild salmon, white fish, pasture raised poultry or eggs, grass fed meat.
Ample amounts of colorful vegetables. Veggies not only have fiber to promote digestive regularity, a key component in detoxification. But they also contain loads of antioxidants called phytonutrients, that help support the immune system and help to inhibit cancer cells. The importance of phytonutrients for cancer prevention is backed by research. The more color you get on your plate, the better. Aim for 2-4 cups with each meal (lunch and dinner).
Limit saturated fat - there is a significant link between saturated fat intake and the development of several cancers, including breast cancer. Saturated fat is largely found in animal products, especially red meat and dairy.
Limit sugar - research suggests a strong link between sugar intake and development of breast cancer, as well as other cancers. Sugar fuels the growth of tumors, and should be limited when possible.
Functional foods for breast cancer:
Flax seeds - Flax is one of the richest forms of lignans, a type of phytoestrogens (plant estrogen) that are protective against breast cancer. Flax is highly susceptible to oxidation and the fats can easily go rancid. Because of this it is best to purchase whole flax seeds, grind them in your high speed blender and store in the freezer. This whole process takes less than 30 seconds. Add 2 tbsp daily to smoothies, juices, apple sauce, yogurt etc.
Mushrooms have many therapeutic applications, and have been shown to have antibacterial, anti-inflammatory, anti-oxidant, antiviral and immune modulating effects on the body. In particular, certain mushrooms have been linked to reduction in breast cancer. Surprisingly button mushrooms are the most common breast cancer fighting mushroom, and is luckily found in grocery stores across North America. I have also included a turkey tail supplement below if you would like additional immune support.
Green tea - EGCG is the active ingredient in green tea that inhibits the growth of breast cancer cells. There is a dose dependent response - the more you drink, the lower the risk. One study recommended five cups of green tea per week, although others suggest a minimum of three cups daily for a truly protective impact. I am admittedly not a huge green tea drinker, and have included green tea extract as part of my supplement protocol (see below) in order to get the therapeutic benefit. Some clinicians have questioned if EGCG interferes with Tamoxifen. A 2020 study found that there’s no interaction between the two, which is a huge benefit for women on tamoxifen who also want to add in EGCG.
Note that foods that are optimal for cancer prevention and that are ideal in remission may vary from dietary focus during active treatment.
Intermittent Fasting
There are many different ways to do intermittent fasting. Like all diets and supplements, intermittent fasting is not for everyone.
However, research does show that it can help to reduce the risk of recurrence for breast cancer survivors. Research has found that a 13 hour fast per night is connected with a 36% reduction in recurrence of breast cancer.
Fasting Mimicking Diet (FMD)
In addition to eating a well balanced diet, I have also begun to weave in the Fasting Mimicking Diet (FMD) a few times per year in order to optimize my metabolic health and help reduce my risk for recurrence.
The only commercially available version of the FMD is through Prolon. The diet is what it sounds like - it’s a five day nutritional program that mimics the benefits of fasting, while still being able to have some food.
The diet is very low in calories - the first day is 1100 calories and the subsequent days are 700-800 calories. It provides the right balance of macronutrients and just enough nutrients to prevent the breakdown of muscle. In addition fasting for a prolonged period of time like this promotes cellular autophagy, which in term also suppresses cancer growth. Emerging research has shown that the FMD supports metabolic changes in breast cancer, associated with long term anti-cancer activity.
I complete a round every 3-4 months as part of my anti-cancer protocol.
Here is a link to get Prolon at a deeply discounted rate.
The FMD is not for everyone, but it can be a valuable tool for many of us, especially for cancer patients and survivors. FMD can be safely utilized during chemotherapy, and studies show that it can help improve the response to chemo treatments as well as reduce side effects.
Supplements for Breast Cancer Prevention
There are many different supplements on the market that vary in quality. Even buying reputable brands on amazon have quality control concerns, therefore I use an online dispensary called Fullscript in order to source the best quality products.
I have included my cancer prevention supplement protocol here so you can see doses and order from a reputable source. Feel free to make a free account and browse the protocols in there. In the spirit of full transparency, please note that I do receive a small kickback for products purchased through fullscript.
High quality multivitamin with activated B complex (I like ones by Thorne, Vital Nutrients and Designs for Health)
Ubiquinol - potent antioxidant
Turkey tail mushrooms - studied for breast cancer prevention
Green tea extract with EGCG - studied for breast cancer prevention
High dose curcumin (from turmeric) - a potent antioxidant
Ground flax seeds - contain protective isoflavones that help reduce breast cancer risk factors
Vitamin D - if levels are suboptimal or low it is essential to supplement with vitamin D to support immune cells in suppressing tumor growth.
Melatonin - is a potent antioxidant that prevents development of tumors, and also sleep and nervous system support.
As a reminder, here is the link to the specific detox support specific supplements I discussed above. Note that there are a few overlapping recommendations!
This post is for educational purposes only and is not intended to be used for medical advice. Any adjunct therapies should be reviewed and approved by your medical team.